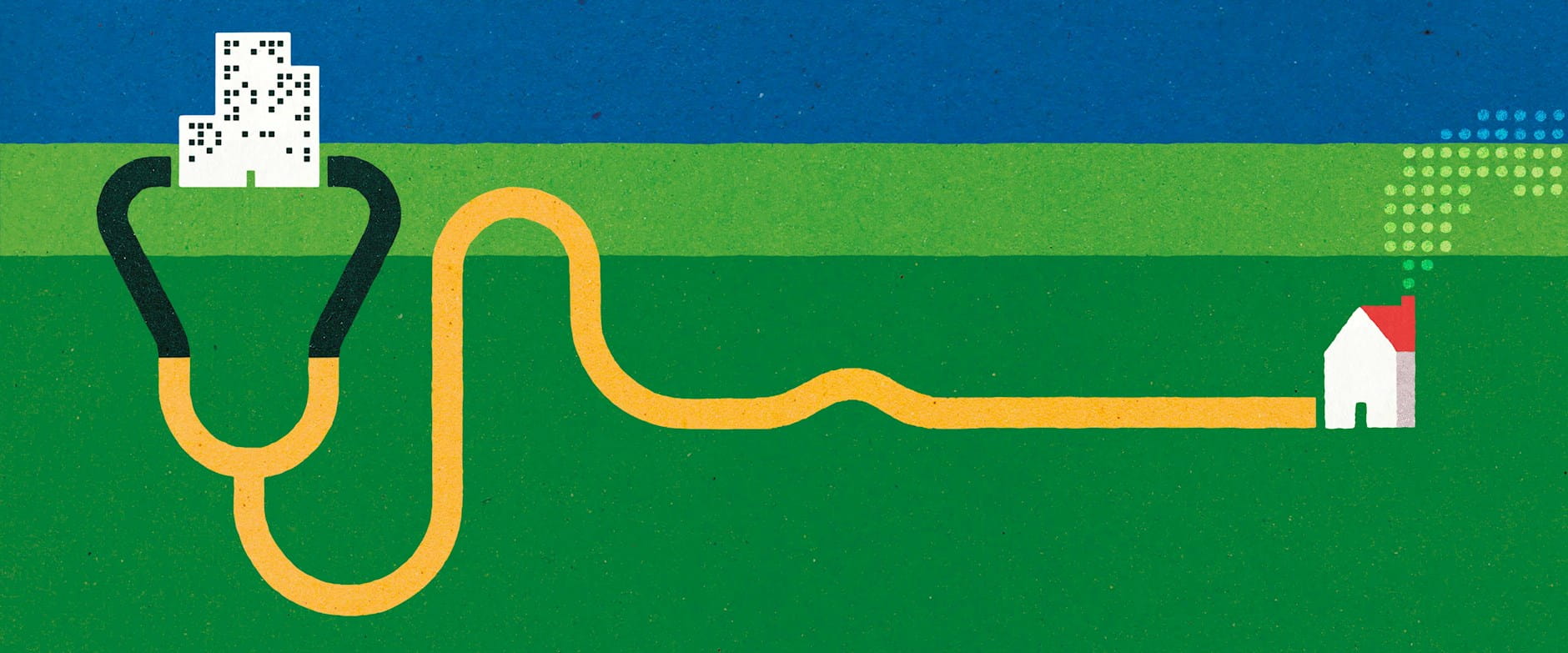
Millions of Americans live far from healthcare services, a problem that’s getting worse as money-losing local hospitals shut down. Before throwing additional billions of dollars at the problem, though, policy makers may want to consider an approach that some research suggests could result in better care at lower cost in many cases.
Rather than investing in putting more medical facilities in remote areas, it could be more effective for the government and private health-insurance companies to pay for patients to visit healthcare facilities, according to Chicago Booth’s Jonathan Dingel, University of Chicago Harris School of Public Policy’s Joshua D. Gottlieb, Harris PhD student Maya Lozinski, and Booth PhD student Pauline Mourot.
“People know that medical tourism is a real thing. But not everyone can afford to travel, and Medicare doesn’t cover it,” says Dingel, referring to the federal healthcare system in the United States for seniors over 65 and people with certain disabilities. “The government could subsidize travel for healthcare.”
Dingel adds some caveats: This wouldn’t apply to urgent or emergency situations. Also, although more women are traveling for care related to high-risk pregnancies and abortions because of recent changes in state laws, childbirth and abortion don’t appear in the Medicare claims data at the same frequency as they do in the general population data. Therefore, the findings don’t fully represent these procedures.
The study analyzed the US healthcare market in terms of transactions between regions. The researchers demonstrate how places such as Rochester, Minnesota, home of the Mayo Clinic, “export” medical services to underserved “importing” areas such as Paducah, Kentucky, as people travel hundreds of miles for care. Such interregional trade accounts for more than a fifth of US healthcare, they find.
Expanded access to medical services through travel
An analysis of 2017 Medicare claims data finds that regions with large markets for medical services—such as that around Rochester, Minnesota—“exported” services to patients from elsewhere, who often sought specialized, high-quality procedures that weren’t available in their home region.
The researchers built a model of the American medical market based on a random sample of 20 percent of traditional Medicare claims from 2017. Medicare is the largest benefits provider in the US, accounting for a fifth of healthcare spending. The sample consisted of 229 million services representing $19 billion of spending.
Trade and market size play a greater role in less common procedures, the researchers suggest. Rural locations tend to have worse health outcomes and fewer doctors per capita. Large urban areas tend to have more specialists who can offer better outcomes based on lots of practice. An area producing 10 percent more of a given service because of greater demand delivers 6 percent higher quality, according to the researchers’ estimates.
“Doctors performing rare procedures export their services more often and across a broader geographic scope,” they write. Consider, for example, a relatively rare cardiac procedure, the insertion of a left ventricular assist device to restore heart function. Half of those patients traveled from outside a single surgeon’s region, the data indicate. Meanwhile, people traveled for only 15 percent of screening colonoscopies, which are routinely practiced and widely available.
Arguing that expanded interregional trade in medical services would give more patients access to the benefits of scale, the researchers contrast the effects of increasing healthcare payments to providers with subsidizing travel for treatment. They find that higher medical payouts in more sparsely populated areas could help expand the local availability of services. But reimbursing patients for travel could expand access to healthcare even more and help improve the quality of services available to people outside major population areas, according to the analysis.
This would be an imperfect solution, though, because people in lower socioeconomic groups are significantly less likely or willing to travel for healthcare, the researchers find. Consequently, larger travel subsidies would be required to even out access across groups of patients. In Paducah, for example, those with the lowest incomes would need a 10 percent larger travel subsidy than those with the highest incomes to achieve the same improvement in access to services, according to the study.
Jonathan Dingel, Joshua D. Gottlieb, Maya Lozinski, and Pauline Mourot, “Market Size and Trade in Medical Services,” Working paper, March 2023.
Your Privacy
We want to demonstrate our commitment to your privacy. Please review Chicago Booth's privacy notice, which provides information explaining how and why we collect particular information when you visit our website.