States Could Save Lives by Sharing Ventilators with Each Other
- By
- April 30, 2020
- CBR - Public Policy
The expected shortage of mechanical ventilators needed to meet the demand from severely ill COVID-19 patients in the United States has prompted the federal government to lean on private industry to dramatically increase the supply. But ramping up production of complex medical equipment in manufacturing facilities configured for other products will take time that many patients don’t have. Research from Chicago Booth’s Dan Adelman suggests there may be another way to make up a portion of any shortfall in ventilator availability: share them between states.
Because the COVID-19 caseload peaks at different times in different states, Adelman argues that policy makers and health officials have an opportunity to maximize the usefulness of each machine by making sure it’s in the right place at the right time. He developed a model that generates a plan for how states could do this—a proof of concept that he says could potentially save lives in this pandemic, but also be applied to a future one.
To project demand for ventilators, Adelman used predictions generated by the University of Washington’s Institute for Health Metrics and Evaluation, which include state-by-state estimates of when, and how high, peak intensive-care occupancy will be. Existing research indicates the US’s current supply of ventilators is around 70,000, roughly 9,000 of which are part of the Strategic National Stockpile.
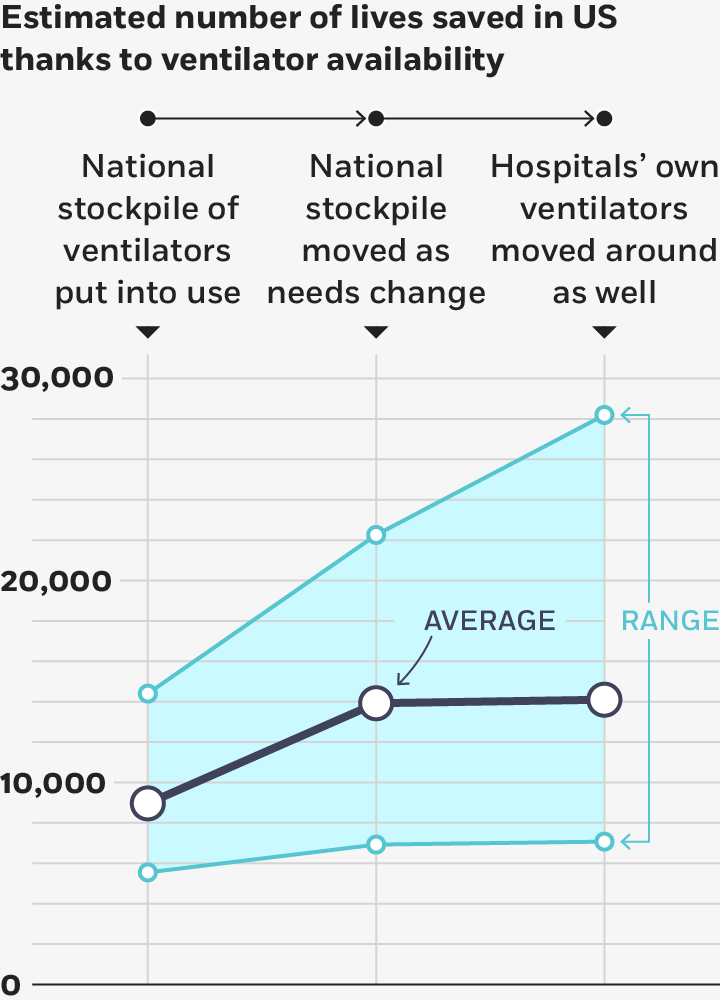
Sharing can help reduce a shortfall
How many lives are saved depends on policy choices and demand for ventilators.
Adelman, 2020
Using these estimates, Adelman modeled a number of scenarios involving high, low, and average levels of demand, as well as various policy choices. He finds that if the ventilators in the stockpile are not deployed at all, the result would be almost 27,000 deaths due to lack of available ventilators, if demand is as expected. The likeliest policy scenario, in which the federal government distributes the ventilators in the stockpile once, and does not reallocate them over time as needs change, saves about 9,000 lives under the same demand conditions, but still leaves 18,000 lives lost due to insufficient availability of ventilators.
If the federal government were to coordinate the sharing of ventilators among states—even if it circulated just the strategic-stockpile ventilators—it could potentially save about 5,000 additional lives under average demand conditions, and far more if demand for ventilators is on the high end of the projections. In the worst-case scenario (the one with the highest demand), coordinated sharing of all ventilators—those in the stockpile and those owned by hospitals—between states would save about 14,000 more lives than a one-time distribution of the stockpile ventilators. In the best-case scenario, sharing all ventilators among the states would result in there being fewer than 1,000 deaths due to ventilator shortage.
Getting states to give up ventilators could be difficult, Adelman acknowledges, as few officials want to risk losing access to essential equipment before the local need for it has abated. He built into his model the condition that no state would part with ventilators until after its COVID-19 cases have peaked, and therefore its need for ventilators has begun to decline.
Adelman cautions that the accuracy of the IHME projections has been called into question. Any deviation between the predicted and actual course of the pandemic would affect how many patients might benefit from ventilator sharing. But, Adelman says, the federal government incorporates the IHME projections into its analyses, therefore it should also adopt this model to minimize lives lost. The analysis also relies on important assumptions about mortality and duration of ventilatory support.
The actions of policy makers and other officials thus far in the pandemic suggests such cooperative action is plausible. Oregon and California have both sent ventilators to other states in order to help shore up supply, and on April 14, President Donald Trump announced a program to allow hospital systems to share ventilators with each other. However, as of its announcement, that program comprised just 4,000 of the roughly 62,000 hospital-owned ventilators in the US.
Adelman calculates that the national stockpile of devices is far too low and should be at least quadrupled for the COVID-19 pandemic. And he notes that coordinating the sharing of ventilators, particularly if it involves the country’s entire stock, is an enormous logistical feat. Under the worst-case demand scenario, it could involve more than 18,000 ventilator moves. But, he writes, “the US military has the requisite expertise: this is really not too different from optimizing and coordinating the movement of tanks and other equipment on the battlefield.”
Dan Adelman, “Thousands Of Lives Could Be Saved In The US During The COVID-19 Pandemic If States Exchanged Ventilators,” Health Affairs, April 2020.
Your Privacy
We want to demonstrate our commitment to your privacy. Please review Chicago Booth's privacy notice, which provides information explaining how and why we collect particular information when you visit our website.